No One Should Have to Live Like This: Steve’s Nine-Year Wait for Freedom
Thousands of people with disabilities in the U.S. use Medicaid to get the supports and services they need to live and be healthy every day. But, people with disabilities must often wait several years to get access to the type of supports they want and need in their own homes. Many are forced into nursing homes and institutions to get the services they need.
But this comes at a critical cost: freedom.
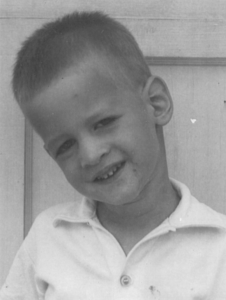
Meet Steve
 Steve has cerebal palsy. For most of his young life, and like many people with disabilities, he lived with his mom. When Steve was only 22 years old, his mom became very ill. Because she could no longer provide the supports he needed, Steve was forced to move into a nursing home to get the care he could no longer receive in his childhood home. Even though Steve knew he could make it in the community with the right supports, he was forced to make this move. This was because his family was concerned about his well-being if he lived independently, and because they feared the appropriate supports were not available to him.
Steve has cerebal palsy. For most of his young life, and like many people with disabilities, he lived with his mom. When Steve was only 22 years old, his mom became very ill. Because she could no longer provide the supports he needed, Steve was forced to move into a nursing home to get the care he could no longer receive in his childhood home. Even though Steve knew he could make it in the community with the right supports, he was forced to make this move. This was because his family was concerned about his well-being if he lived independently, and because they feared the appropriate supports were not available to him.
The nursing home put Steve in the long-term Alzheimer’s unit with people who were often in their 80s and 90s. This was not Steve’s choice. Steve was placed in an available bed where all long-term residents were put.
Steve hated living in the nursing home and often felt like the care he got from staff was lacking.
“I had to wait an hour for someone to respond when I asked for help. Sometimes, the nurses would come in and turn the call light off instead of helping me. I was always the last to be fed. When I needed to go to the bathroom, I would wheel my chair out to the hall and tell the staff—but they would walk away. I had to fight with the nurse to get medications. If I told someone I wasn’t getting taken care of, the care would be worse because the staff would get mad at me. At night, I couldn’t sleep because the other residents were screaming or because staff were buffing the floor.”
After a year in the nursing home, Steve’s case manager got him on the waiting list for Medicaid home and community-based services (HCBS). Access to HCBS would allow Steve to move out of the nursing home and get the help he needed in his own home in the community.
“I spent eight years on the waiting list… Every year, I got a letter about where I was on the waiting list. Every time I got that letter, I was so discouraged and disappointed because it felt like my name was not coming up. And, I thought that I would never get out.”
Finally, after nine years in the nursing home, Steve’s name did come up, and he got out.
“On my last day in the nursing home, I went to the administrator and told her, ‘thank you for kicking me out—you made my wish come true.’ When I got out and got [HCBS services], I finally had the freedom to do what I wanted to do… I could eat when and what I wanted—and the food was actually warm. I could sleep better at night. I could use the bathroom when I needed to. I could go out with friends without having to come back at a certain time. I did not have to fight nurses to get my medication. I had freedom—and a life like yours.”
Now, Steve lives independently in his own home in the community, with support from paid caregivers. While he does still experience challenges with things like getting transportation services, finding safe and affordable housing, and finding paid caregivers, he believes he is where he belongs.
Steve’s nine years in a nursing home profoundly impacted him and he wants to make sure no one has to live the way he had to.
“Just because we are disabled, [doesn’t mean we don’t deserve] equal rights—we do not belong in an institution. We should have the same opportunities as anyone else. Everyone should get the help they need in their home, [and everyone should have the right to live the life they want].”
To others with disabilities, Steve offers these words of encouragement.
“People will say there are no other options for you in your area besides an institution…Do your research. Have a backbone, be tenacious, and don’t ever give up. You are always going to have roadblocks—but you have to find your way past them. You can do it.”
Check out this video to learn more about the role of Medicaid HCBS and Supplemental Security Income in Steve’s and other advocates’ lives.
This injustice must end.
No one should have to give up their freedom to get the services they need. The Arc works every day:
- To make sure people can get the Medicaid HCBS they need
- To end long waiting lists for HCBS services
- To close institutions, which still exist in 36 states nationwide
Join us! Visit thearcwebdev.wpengine.com/MedicaidCantWait to learn more and see how to advocate for HCBS with us.


 There were no supports available outside of the public schools and the schools were not prepared to serve children with high levels of need. When my brother was kicked out of school at a very young age (before the federal law ensuring a right to education) for his disability-related behaviors, he had nowhere to go except home all day with a very loving caregiver. He missed the routines and rhythms of school and had a hard time staying home while everyone else went to work or school daily. He waited all day for the staggered returns of kids and parents, dinner, and then his beloved ride to the drugstore for a Coke and a long drive listening to rock and roll and beach music on the radio. Jud also had daily trips to the Post Office with our Dad to pick up the mail for his business, trips to the barbershop, church on Sundays, other local gathering places, and a house full of our friends and exchange students who lived with us at various times. He loved all the interaction and was known all over town.
There were no supports available outside of the public schools and the schools were not prepared to serve children with high levels of need. When my brother was kicked out of school at a very young age (before the federal law ensuring a right to education) for his disability-related behaviors, he had nowhere to go except home all day with a very loving caregiver. He missed the routines and rhythms of school and had a hard time staying home while everyone else went to work or school daily. He waited all day for the staggered returns of kids and parents, dinner, and then his beloved ride to the drugstore for a Coke and a long drive listening to rock and roll and beach music on the radio. Jud also had daily trips to the Post Office with our Dad to pick up the mail for his business, trips to the barbershop, church on Sundays, other local gathering places, and a house full of our friends and exchange students who lived with us at various times. He loved all the interaction and was known all over town.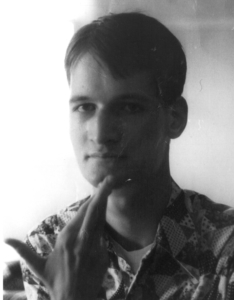 Sadly, as each of his older siblings began to leave home for college, military service, or otherwise, Jud’s physical size and his inability to control his frustrations and emotions became dangerous for our aging parents. After much searching and trying many approaches, the only available service for someone with his needs was the state institutional system. This was devastating for Jud, for our whole family, and for the many friends who had known him over the years. Jud suffered greatly from the travel distance from his family (even though we visited regularly), home and hometown, friends, and routines. And while there were some wonderful staff who supported him in his new location, we were horrified to learn that he also suffered some terrible abuses– the kinds of things that can be hidden when people who are unable to communicate or be understood cannot tell others what is happening to them. My father found that Jud had been burned with cigarettes and that other men in his unit had been more extensively burned. In other incidents, men in his unit died after being subjected to dangerous restraint methods. He also suffered from toxic environmental conditions, including asbestos and sewage leakage. As a family, we were determined to end these abuses.
Sadly, as each of his older siblings began to leave home for college, military service, or otherwise, Jud’s physical size and his inability to control his frustrations and emotions became dangerous for our aging parents. After much searching and trying many approaches, the only available service for someone with his needs was the state institutional system. This was devastating for Jud, for our whole family, and for the many friends who had known him over the years. Jud suffered greatly from the travel distance from his family (even though we visited regularly), home and hometown, friends, and routines. And while there were some wonderful staff who supported him in his new location, we were horrified to learn that he also suffered some terrible abuses– the kinds of things that can be hidden when people who are unable to communicate or be understood cannot tell others what is happening to them. My father found that Jud had been burned with cigarettes and that other men in his unit had been more extensively burned. In other incidents, men in his unit died after being subjected to dangerous restraint methods. He also suffered from toxic environmental conditions, including asbestos and sewage leakage. As a family, we were determined to end these abuses. Jud’s experiences fueled my passion to change the system. I worked in Washington to pass federal legislation to move the Medicaid funding bias away from institutions and to build the community service system, making the community the preferred service setting. My advocacy led me to a career in The Arc’s national public policy office, which I joined in 1984. While our systems have evolved since the 70s through the late 80s when my brother was experiencing so much pain, we still have a long way to go. I am happy to report that Jud was eventually able to leave the state institution and live in a group home about 7 minutes from our widowed mother in his beloved hometown for the last 20+ years of his life. Jud also experienced some serious problems in his group home, but those were able to be discovered and remedied because family were nearby and able to observe how he was doing. For those who understood him, Jud continued his mantra: “Stay at the new house; not gonna keep saying it” throughout those years, lest anyone think he would ever want to go back to the institution.
Jud’s experiences fueled my passion to change the system. I worked in Washington to pass federal legislation to move the Medicaid funding bias away from institutions and to build the community service system, making the community the preferred service setting. My advocacy led me to a career in The Arc’s national public policy office, which I joined in 1984. While our systems have evolved since the 70s through the late 80s when my brother was experiencing so much pain, we still have a long way to go. I am happy to report that Jud was eventually able to leave the state institution and live in a group home about 7 minutes from our widowed mother in his beloved hometown for the last 20+ years of his life. Jud also experienced some serious problems in his group home, but those were able to be discovered and remedied because family were nearby and able to observe how he was doing. For those who understood him, Jud continued his mantra: “Stay at the new house; not gonna keep saying it” throughout those years, lest anyone think he would ever want to go back to the institution.








